Cerebral Palsy
What is cerebral palsy (CP)?
Cerebral palsy (CP) is a term used to describe a group of chronic conditions affecting body movement and muscle coordination. It is caused by damage to one or more specific areas of the brain, usually occurring during fetal development; before, during, or shortly after birth; or during infancy (see below). Thus, these disorders are not caused by problems in the muscles or nerves. Instead, faulty development or damage to motor areas in the brain disrupts the brain's ability to adequately control movement and posture.
Cerebral refers to the brain and palsy to muscle weakness/poor control. Cerebral palsy itself is not progressive (i.e., brain damage does not get worse); however, secondary conditions, such as muscle spasticity, can develop which may get better over time, get worse, or remain the same. Cerebral palsy is not communicable. It is not a disease and should not be referred to as such. Although cerebral palsy is not curable in the accepted sense, training and therapy can help improve function. CP in United States affects approximately 760,000 individuals. Source: UCP Foundation
Why use the name cerebral palsy?
Some parents strongly object to the term cerebral palsy because they feel it carries negative connotations about their child and that it enforces lowered expectations for their potential. For example, it might be that a person called mentally retarded will be treated in accordance with the stereotype evoked by the term. We understand and agree with this concern. However, in this website we have chosen to retain the term CP because it is the most specific clinical description to use with the public at large and parents less familiar with infants with neurological injury.
Are some causes of CP preventable?
Although we lack neuro-repair treatments for patients with already established CP, there are some cases in which we think that medical intervention could prevent CP from occurring. Even so, for many types of neurological injury in infants, no preventative therapy is available; further research is desperately needed to create therapeutic options. For more information on this, see the Newborn Brain Research Institute (NBRI)
But what can be done today? One very important aspect of prevention is good prenatal care, which can predict and limit conditions in which oxygen to the fetus is impaired. A second way to prevent CP in some babies is expert resuscitation. Rates of CP in the United States declined by half when doctors specially trained in neonatal resuscitation (neonatologists) began to practice in hospitals around the country.
Figure 1
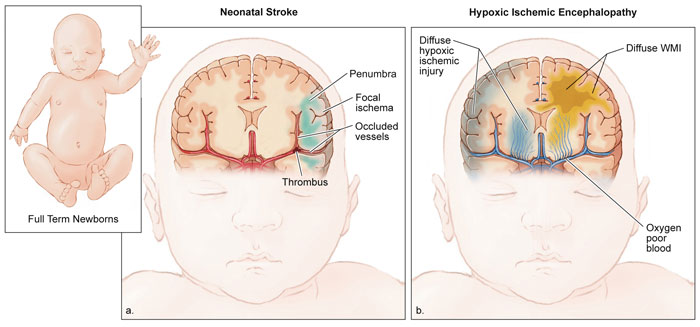
Another recent advance has been development of hypothermia in which the body and brain are cooled down to about 92°F (33.5°C), as opposed to the normal body temperature of 97.8°F (37°C). Hypothermia is appropriate for some full-term babies that have been deprived of oxygen around the time of birth (a condition called Hypoxic-ischemic Encephalopathy (HIE); see Figure 1A, and has been shown to prevent very severe brain damage that can lead to death.
Neonatal stroke is also associated with lack of oxygen to the brain in full-term infants (Figure 1B). When this injury happens at the time of birth it can also probably be helped by hypothermia. The William H. Tooley Intensive Care Nursery at UCSF Benioff Children's Hospital participated in early research in this therapy and began to routinely provide this treatment in 2007.
Preterm infants typically suffer from two other causes of brain injury that probably result from the delicate nature of the developing human brain. Intraventricular Hemorrhage (IVH) refers to bleeding in the brain and is graded from grade 1 (mild) to grade 4 (severe).
Figure 2
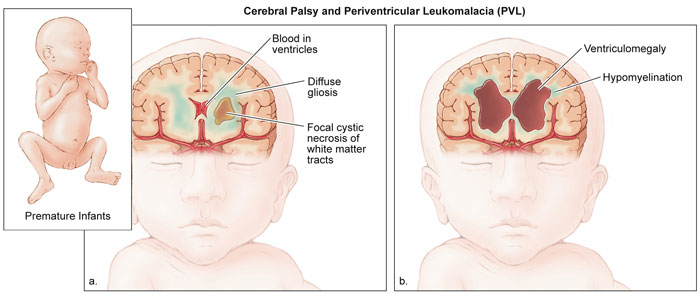
Figure 2A shows a severe IVH with bleeding into the cavity in the center of the brain called the ventricles and also the brain tissue. Another injury seen in preterm infants is called Periventricular Leukomalacia (PVL). This affects white matter tracts of the brain that carry messages between nerve cells of the brain and body. PVL can cause severe neurological problems with movement.
All the conditions described above can cause either mild or very severe brain damage that can lead to death. Each case requires careful evaluation by doctors specialized in assessing neurological injury in babies. To advance the level of care for infants with such injuries, the William H. Tooley Intensive Care Nursery at UCSF Benioff Children's Hospital began the worlds first Neuro-Intensive Care Nursery (NICN)